ฟิลเลอร์ถุงใต้ตาเปลี่ยน “ถุงใต้ตา” เติมเต็มความมั่นใจ

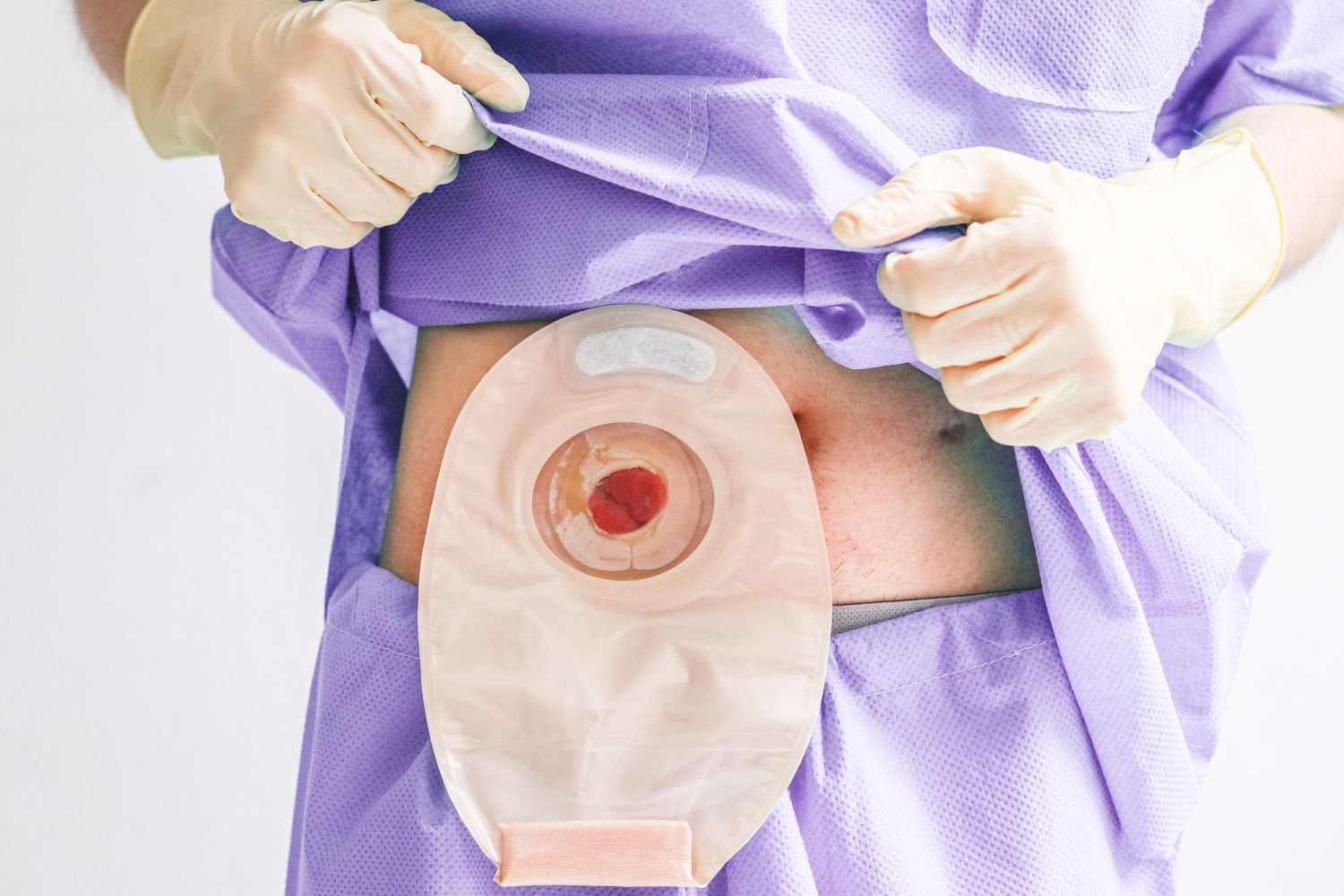
ใต้ตาคล้ำ มีถุงใต้ตา ตาลึก ตาโหล… สารพัดปัญหาที่สร้างความกังวลใจให้กับหลายคน ไม่ว่าจะเป็นผู้หญิงหรือผู้ชาย ทำให้ใบหน้าดูมีอายุ และดูไม่สดใสเหมือนเดิม การทำฟิลเลอร์ถุงใต้ตา จึงเป็นวิธีแก้ปัญหาที่ปลอดภัยและกำลังได้รับความนิยม แต่ในขณะเดียวกัน ก็ยังมีอีกหลายคนที่ยังไม่เข้าใจว่า การทำฟิลเลอร์ที่ถุงใต้ตาคืออะไร เหมาะกับใครบ้าง และอยู่ได้นานไหม วันนี้เรามาหาคำตอบเหล่านี้ไปพร้อม ๆ กันเลยดีกว่า ฟิลเลอร์ถุงใต้ตาเหมาะกับใครบ้าง การทำฟิลเลอร์ถุงใต้ตาเป็นการฉีดสารเติมเต็ม ที่เรียกว่า กรดไฮยาลูโรนิค ซึ่งเป็นสารที่มีอยู่ในผิวเราอยู่แล้ว จึงมีความปลอดภัย เพราะร่างกายของเราสามารถสลายกรดไฮยาลูโรนิคออกไปได้เอง การฉีดเข้าไปใต้ผิวหนังบริเวณใต้ตา ซึ่งเป็นหัตถการที่ไม่ทำให้เกิดแผล เพื่อทำการเติมเต็มร่องลึก ลดเลือนถุงใต้ตา ทำให้ใต้ตาดูเต่งตึง